Best Foods to Lower Blood Sugar & Lose Weight With Insulin Resistance
Jan 26, 2022What if I told you that following the Diabetes Plate method advocated by the American Diabetes Association is not the best way to reverse prediabetes or diabetes?
My hope is that this episode brings crystal clarity about the best foods to eat to lower blood sugar (and why). Foods that keep blood sugar low, will also help keep blood insulin (which is your fat creation and storage hormone) low.
If you’re among the estimated 88% of adults with insulin resistance, these are also the best foods to help you lose weight with insulin resistance.
Listen to This Episode
What Is Prediabetes?
Prediabetes is when your blood sugar is elevated, but not high enough to be considered in the diabetes range.
Normal fasting blood glucose is 70 to 99 or an A1c of 5.6 or less.
Prediabetes is when your fasting blood glucose is 100 to 125 or an A1c of 5.7 to 6.4.
Type 2 diabetes is when your fasting blood glucose is 126 or higher on two separate tests, or an A1c of 6.5 or greater.
Another test that’s a little more involved than the fasting blood sugar or A1c test is the Oral Glucose Tolerance Test, or OGTT.
Glucose tolerance refers to how well your body processes glucose - or sugar - after being given a measured dose, usually 75 grams, orally. 75 grams of glucose is the equivalent amount of sugar that would be in almost 2 cups of pasta or 1 and ¾ cups of white rice.
Normally what happens when you have a bolus of glucose like this, is your blood sugar goes up, and comes back down over the next several hours. But if you have prediabetes or type 2 diabetes, your blood sugar takes longer to come back down.
Here are the cutoffs for the oral glucose tolerance test 2 hours after consuming 75 grams of glucose.
A blood glucose under 140 milligrams per deciliter is considered normal.
A blood glucose of 140 to 199 milligrams per deciliter indicates you may have prediabetes.
A blood glucose of greater or equal to 200 milligrams per deciliter indicates you may have diabetes.
What Is Insulin and How Does Insulin Resistance Develop?
Insulin is the hormone that helps allow blood glucose to move from your blood into your cells. Your pancreas can only produce so much insulin. Over time the amount of insulin required to keep your blood sugars normal goes up and up.
With the rising levels of insulin in your blood, your cells become resistant to its effect. So it’s this upward regulation where your blood sugars go up after a meal, the normal amount of insulin is released but your cells are less sensitive to insulin’s effect because of the insulin resistance.
So more insulin is secreted to keep blood sugars in the normal range.
But over time, you become more and more resistant, and your pancreas reaches its capacity at how much insulin it can produce. Insulin can no longer keep blood sugar down. That’s when we start to see prediabetes.
What Is the Kraft Test and How Does It Detect Pre-Pre Diabetes
Dr. Pradip Jamnadas talks about the Kraft test, which is a combination test that measures both the glucose and insulin response following a meal.
The Kraft test can catch prediabetes even before your blood glucose level, because it tests the insulin in the background that’s actually responsible for controlling your blood glucose.
High insulin levels are associated with all the same conditions as type 2 diabetes - things like cardiovascular disease, osteoporosis, dementia, inflammation, blindness, and peripheral neuropathy.
For the Kraft test, you drink 75 grams of glucose. Then your glucose and insulin are measured at the half hour, 1, 2, and 3 hour marks to make the curves and see the relationships between your glucose and insulin response.
A prediabetic could still have a relatively normal blood glucose response. In people with a healthy insulin response, you should see the insulin curve following the blood glucose curve.
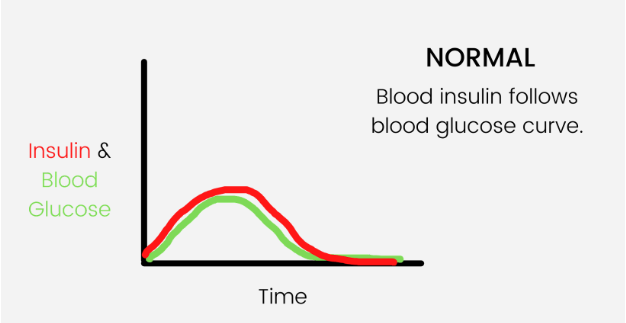
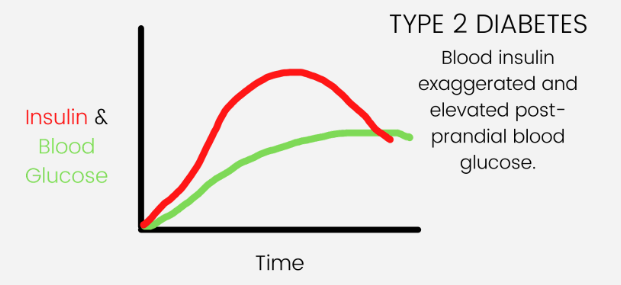
But in someone who has prediabetes, the insulin curve will be higher because more insulin is needed. This is because the cells are less sensitive to insulin’s effect. Their body is a little insulin resistant, but their insulin can still keep up and that brings the sugar level down.
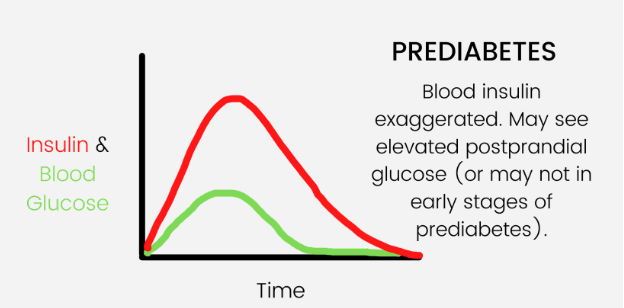
But eventually their body won’t be able to make enough insulin to keep up and they will have impaired fasting glucose - or prediabetes. Left untreated, prediabetes can develop into type 2 diabetes with both elevated glucose and insulin levels.
This 2017 research study backs this claim up and says that “using fasting glucose, oral glucose tolerance test (OGTT) or A1c may not be the most effective early screening tool for T2D."
Incorporating fasting insulin and especially insulin after an oral glucose tolerance test as enhanced screening methods, may help to increase the ability to detect diabetes and prediabetes, allowing earlier intervention to prevent diabetic complications.”
Symptoms of Prediabetes & Insulin Resistance
Most pre-diabetics also struggle with weight gain, or at least poor body composition (lower muscle mass and higher fat mass.) This is because insulin is the primary hormone responsible for our body weight.
A rise in fat mass is a direct cause of insulin resistance because insulin is the hormone responsible for making adipose (fat) tissue.
Then this fat releases a hormone called leptin. Over time as your insulin goes up, your fat goes up, and your leptin goes up. You become resistant not only to insulin but also leptin.
Leptin works to counteract the effects of ghrelin - or your hunger hormone. So the negative feedback loop that is supposed to keep you at a healthy weight becomes broken.
Leptin stops inhibiting ghrelin, so you sense hunger and eat, even though you have plenty of fat for fuel on your body.
The best way to fix this and restore a healthy body fat and weight is to start at the source - lower insulin resistance.
You’ve heard the phrase when the tide comes in all the boats rise? Well in our body, insulin is the tide. When we focus on lowering insulin, all your other risk factor numbers improve.
Triglycerides go down. Blood pressure goes down. HDL cholesterol goes up. Glucose goes down. Body fat comes down, especially the unhealthy visceral belly fat that’s inflammatory.
When we are looking at hidden symptoms of prediabetes, what we are actually focusing on are the hidden symptoms of insulin resistance and elevated blood sugars - because that is what’s driving your diabetes.
According to the Centers for Disease Control (or CDC), approximately 88 million American adults—more than 1 in 3—have prediabetes.
Of those with prediabetes, more than 84% don't know they have it. So it’s safe to say the most common symptom of prediabetes would be no symptoms at all...at least none they recognize as being related to prediabetes...but they are!
- One symptom of prediabetes is weight gain, specifically a gain in fat mass. Your insulin is not only responsible for regulating blood sugars, but also your weight.
- Excessive hunger can also be a symptom of prediabetes - especially carb and sugar cravings. Cells that are resistant to insulin will sense a bit of starvation and increase your hunger - especially for foods that are known to give quick energy - the refined carbs.
- Excessive thirst can be a symptom of prediabetes.
- This increased fluid intake can also cause increased urination, which can be another symptom of prediabetes.
- Elevated blood pressure is a common symptom of prediabetes. High insulin directly causes high blood pressure. For some, high blood pressure may be the first sign of insulin resistance or prediabetes, they just may not have heard of this link before.
- Fatigue is a common symptom of prediabetes. There are a lot of different potential causes for this fatigue, but a major one are the blood sugar spikes and dips that result from grazing on carbs. Your body is using a lot of energy just trying to balance your blood sugars.
- Other symptoms of high blood sugar are blurred vision or numbness and/or tingling in your hands and/or feet. This is called peripheral neuropathy and it can be very painful and limit activity.
- Frequent infections are another sign of prediabetes. High blood sugar impairs the white blood cell function critical to a healthy immune system. And sugar is a great source of energy for invading bacteria and fungi. These factors increase the risk of infections of all kinds and impair the immune system so it takes longer to heal.
- Upper respiratory infections and urinary tract infections are two of the more common infections. If you notice that you’re getting them more often - consider that a warning sign to check your blood sugar and get them under control if you need to.
- In line with this impaired immune response would be slow healing wounds. That’s why people with diabetes - especially those with peripheral neuropathy who may not be able to feel well - must be vigilant about visually inspecting their feet for cuts to catch and treat them early.
- Diabetic foot wounds can be very hard to heal and lead to amputations of toes, or unfortunately sometimes their foot or part of their leg.
- The last symptom I cover in this episode is brain fog or confusion. Your brain is sensitive to insulin, too. In fact, Alzheimer’s disease is now being called type 3 diabetes. So for those of you who are motivated to keep your cognitive health as you age, I hope knowing there is a strong association between diabetes and dementia gives you strong, sustained motivation to prioritize your health.
Especially around menopause as estrogen drops - which causes insulin resistance to go up - you’re going to be at an increased risk of developing prediabetes or progressing into diabetes. So the years surrounding menopause are an especially critical time in a woman’s life to get blood sugars under control.
Takeaway #1 to Lower Blood Sugar: Stop Counting Points and Calories
I cannot emphasize enough how important it is to stop counting points or calories to get healthy. They are arbitrary numbers. There are no points or calorie receptors on your cells. There is - however - an insulin receptor in every cell.
Takeaway #2 to Lower Blood Sugar: Start Tracking Macronutrients
In order to understand the best foods to lower blood sugar, it’s much more beneficial to learn how to track your macronutrients.
When you’re counting calories or points, you’re actually disincentivized to eat foods that are high in calories - which happen to be some of the best foods to help lower blood sugar and lose weight.
Carbohydrates (specifically starch and sugar) and proteins have 4 calories per gram, whereas fat has 9 calories per gram. The problem arises when you look at this chart for how different macronutrients impact insulin (and thus blood glucose).

Fat actually has the lowest insulin response, protein has a moderate, starches and sugars have the highest. Fiber actually slows the digestion of your food meaning it slows the glucose and insulin response.
Protein was covered extensively in this episode: How to Get More Protein While Using Intermittent Fasting to Lose Weight. Check it out to learn more about how adequate protein can be great for weight loss and healthy blood sugar levels.
You could eat a bowl of low-fat oatmeal and think you’re on the right track, when in reality you’d be a lot better with an omelette. Counting points or calories doesn’t show you this, but tracking macros does.
Takeaway #3 to Lower Blood Sugar: Limit Your Intake of Refined Starches and Sugars and Replace Them With Lower-Carb Options
That would include whole grain and multi-grain products, too. If you love bread, pasta, rice, and sweets, there are healthier low-carb alternatives that still taste great.
Is whole wheat healthier than white?
Yes, but at that point you're kind of cutting hairs - they are still both high in carbs. You’re better off to reduce your portion size, or replace it with a food that’s higher in fiber, protein, or fat.
What I’ve done with my diet is find substitutions that are either less processed or even better, made with higher fat flours like coconut flour or almond flour.
For example, instead of white pasta, we like the Banza chickpea pasta. A side-by-side comparison of their macronutrient breakdown on the Carb Manager App shows you why.
2 ounces of dry, white pasta has 41 grams of net carbs, 7 grams of protein, and 1 gram of fat.
2 ounces of pasta made from chickpeas has 27 grams of net carbs, 13 grams of fiber, and 4 grams of fat.
When we have spaghetti, I’ll do a big serving of the meat sauce, and a smaller serving of chickpea noodles.
Another example of a time where I don’t find a substitution is when we make quick steak sandwiches. For these, I’ll just scoop out my white roll as much as I can. That’s an easy way to reduce your portion size of bread while still enjoying a bun.
Little swaps like this can be really helpful for living a low insulin lifestyle that doesn’t feel restrictive like you have to give up your favorite foods.
Look at the food label and check to see if it’s high in net carbs, and particularly if it’s high in added sugar. If it is - find an alternative.
Using the Carb Manager or another macros tracking app can make this even easier to visualize.
Our members and clients are often shocked when they see how many carbs they are actually eating. Once they start to bias their food intake more towards protein and fat, they feel better and start seeing weight loss.
Examples of high starch and sugar foods that will raise your blood sugar are cereals, bread, pasta, bagels, chips, and tortillas made with flours high in starch such as wheat, rice, potato, oat, bran, sorghum, barley, millet, corn, and the like.
Also consider foods with sugar in them like high sugar fruits, candy, donuts, cake, cookies, ice cream, brownies, pop, sweetened iced tea, many sports drinks, many foo-foo coffee drinks like Frappuccino's, and some of those “healthy” kombucha drinks.
For example, a large (12 ounce) white chocolate mocha from Starbucks has 40 grams of sugar - which is about as much as a can of Pepsi!
Added sugar is also hiding in drink additives like coffee creamer. My favorite used to be the Peppermint Mocha creamer and I had about 2 cups a day with 2 tablespoons of creamer in each.
There is 5 grams of added sugar in 1 tablespoon so I was having 20 grams of added sugar just in my coffee each morning!
Now you may be wondering if sugar-free creamer is any better. My answer is no and that brings me to our fourth takeaway.
Takeaway #4 to Lower Blood Sugar: Avoid Sugar-Free Ingredients That Still Raise Blood Sugar
Now while macronutrients are important, they don’t tell the full story. A food may have zero carbs or calorie, and still impact blood sugar.
This is where it becomes important to screen packaged foods for a few key ingredients to avoid.
Here are the main artificial sweeteners and texture additives to look out for on the ingredients list: maltodextrin, sucralose, saccharin, aspartame, and acesulfame potassium.
If it has these, steer clear because chances are this sugar-free product will still raise your blood sugar.
The first ingredient is maltodextrin. Maltodextrin is a white powder made from corn, rice, potato starch, or wheat. Even though it comes from plants, it's highly processed. I did a little research into maltodextrin and was a little grossed out by what I found.
Maltodextrin is used as a thickener or filler to increase the volume of a processed food. It’s also used as a thickener in personal care items such as lotion and hair care products.
It’s also a preservative that increases the shelf life of packaged foods. It’s inexpensive and easy to produce, so it’s useful for thickening products such as instant pudding and gelatins, sauces, and salad dressings.
Here are a few examples of common foods that contain Maltodextrin: sugar-free jello, sugar-free jam, Crystal light and many other similar pouches you add to water.
It can also be combined with artificial sweeteners to sweeten products such as canned fruits, desserts, and powdered drinks.
Maltodextrin has an even higher glycemic index than table sugar! This means that maltodextrin can cause a sharp increase, or spike, in your blood sugar shortly after you eat foods that contain it.
The other sugar-free ingredients I want you to look out for are the artificial sweeteners saccharin (a.k.a. Sweet‘N Low), sucralose (a.k.a. Splenda) aspartame (a.k.a. NutraSweet and Equal), and acesulfame potassium (a.k.a. Ace-K and Sunett).
All of these have been found to raise blood sugar levels by dramatically changing the makeup of your gut bacteria. These are also known as “post-oral” metabolic effects.
Unlike maltodextrin they may not immediately impact your blood glucose, but over time they will contribute to insulin resistance and poor blood sugar control.
If you’re trying to reduce your sugar intake but still want a healthy sweetener, I recommend sticking to stevia, monk fruit, or erythritol.
Stevia and monk fruit tend to be a little easier on the gut and cause less gas than erythritol.
Key #5 to Lower Blood Sugar: Choose Fats Wisely
When it comes to lowering blood sugar, the good news is that great food actually can help you do this!
Foods rich in healthy fat and protein are very satiating - meaning they help keep you full from one meal to the next. They are also nutrient-dense - meaning unlike carbohydrates that usually just get stored as energy if you don’t need the energy right away, fat and protein are put to use to make hormones, bones, muscles, and more.
I’ve covered the different types of fats in depth in this episode but as a quick review, you’re going to want to bias your fat intake towards whole, unprocessed fats from animals and plants, and avoid the processed fats.
Great sources of fat from dairy would include whole milk, cream or half n half, string cheese, full-fat Greek yogurt, cottage cheese and butter.
I’ve done a lot of research on saturated fats and in my opinion they are neutral at worst, beneficial at best. If you’re worried about eating a lot of saturated fat because you’re afraid of high cholesterol, I’m going to push back on that because saturated fat is one of the few nutrients shown to raise HDL cholesterol which is protective against heart disease.
I’ve done interviews with Dr. Nadir Ali and Nina Teicholz who will hopefully put your mind at ease on this topic.
Dr. Jason Fung does a great job putting the myth that saturated fat is linked to heart disease to bed. He sums it up by saying in his book The Obesity Code,
“Saturated fats raise HDL (the “good”) cholesterol and change LDL from small, dense (bad) to Large LDL, which is mostly benign. Overall, saturated fats do not harm the blood lipid profile like previously believed.” - The Obesity Code
Other healthy high-fat foods that would keep insulin are omega-3 fatty acids, specifically from fatty fish because these are high in EPA and DHA that are anti-inflammatory. Plant sources of omega-3s like walnuts, chia seeds, and flax seeds are higher in ALA.
There is a low conversion rate (about 8-15%) from ALA to EPA and DHA. So if you’re wanting the anti-inflammatory benefits, you’ll need to get the EPA and DHA from fatty fish like tuna, trout, salmon, herring, mackerel, cod, and the like.

If you don’t want to eat fish, you can get it from an algae oil. Be sure to run all supplements by your doctor just like any other medication.
Omega-6 fatty acids found in nuts and seeds are also healthy but omega-6 fatty acids found in the refined oils from those nuts and seeds are not healthy.
This is an important distinction.
Whole food omega-6 is okay. Processed omega-6 is inflammatory.
While they may not directly raise blood sugar or insulin, oils like canola, safflower, corn, soybean, and sunflower oil are not healthy to eat.
The food products like Ranch salad dressing, popcorn popped in this oil, chicken fingers and fries fried in vegetable oil, are not healthy.
You’re much better sticking to olive oil, coconut oil, avocado oil, butter, ghee, or lard for cooking.
The last kind of healthy fat I focus on are omega-9 fatty acids (or monounsaturated fats) from whole foods like avocados, olives, nuts and seeds. These are great for you and help keep blood sugar and insulin low.
Along with the processed omega-6 fatty acid oils, the other unhealthy fat to avoid would be artificial trans fats and foods that contain them. Now there is some naturally occurring trans fat in animals and those are okay.
What I want you to look for are the words “partially hydrogenated.” Partially hydrogenated oil contains trans fat.
In 2015, the Food and Drug Administration (FDA) said that partially hydrogenated oil can no longer be “generally recognized as safe” or GRAS.
They said removing it from food could prevent thousands of heart attacks each year. In 2018 the FDA went a step further and banned trans fats from new food products.
Because of this ban on trans fats, food companies have had to reengineer products. I’ve noticed more “fully hydrogenated” oils on the ingredients list - this is still highly processed and unhealthy.
Some food products may still have trans fats such as margarine, vegetable shortening, microwave popcorn, fried fast foods, bakery products like muffins, cakes, pastries and doughnuts, as they are often made with vegetable shortening or margarine which are high in trans fats.
Non-dairy coffee creamers, some canned frostings, crackers, chips, pies, and pizza depending on their ingredients may also have artificial trans fat.
Takeaway #6 to Lower Blood Sugar: Eat More Protein
As discussed in-depth in this episode, aim for about 1.1 - 1.5 grams of protein per kilogram of body weight a day and have at least 30 grams of high quality protein at each meal to reach about 3 grams of the amino acid leucine, so you can trigger more muscle growth.
Great sources of protein would be cottage cheese, string cheese, beef, chicken, pork, fish and shellfish, soy products such as edamame or tempeh, and quality protein supplements from powders and bars that aren’t full of a bunch of those unhealthy sugar-free ingredients I mentioned that can still raise blood sugar.
Takeaway #7 to Lower Blood Sugar: Optimize Your Micronutrients
Harvard Health has a great table of vitamins and minerals, many of which are needed to optimally metabolize our food. This table also reports the recommended amount of each micronutrient we get each day.
Let’s start with the mineral Magnesium.
One study reported that 25 to 39% of people with diabetes also have a magnesium deficiency.
Their summary was that hypomagnesemia is seen in type 2 diabetes and there is an inverse correlation between the person’s magnesium level and fasting and postprandial blood glucose levels.
This means that those individuals with higher levels of magnesium had lower fasting glucose, and better blood glucose response after a meal.
The study authors suggested that periodic monitoring of magnesium concentration and magnesium supplementation can prevent chronic complications related to diabetes mellitus.
Another study of 42 people with type 2 diabetes found that a magnesium supplement of 250 milligrams per day for 3 months helped reduce insulin resistance and improved blood sugar control.
The next micronutrient to consider is chromium. I found this 2021 Systematic Review and Meta-Analysis on the effect of chromium on blood glucose.
This review included a total of 10 randomized controlled trials involving 509 patients. Its results were a little less thrilling than what I’d hoped.
The “meta-analysis results showed that the differences between the experimental group and the control group in only one indicator of hemoglobin A1c were statistically significant, while there were no statistically significant differences in other indicators. The use of chromium supplements can reduce the A1c of type 2 diabetic patients to a certain extent, but it cannot effectively improve the fasting blood glucose and blood lipid levels of type 2 diabetic patients.”
So you may get a slight benefit with chromium supplement, but I would focus on magnesium first.
Foods high in magnesium are leafy greens, pumpkin seeds, almonds, low sugar dark-chocolate, some types of fish like salmon, mackerel and halibut.
The vitamin D family is also essential to ward off insulin resistance and improve your blood sugar regulation. Great natural sources of vitamin D include fatty fish (like tuna and salmon), egg yolks, cheese, and fortified milks.
In Why We Get Sick, Dr. Bikman also identifies cysteine, calcium (or more specifically dairy), and zinc as important micronutrients to help with insulin resistance.
So while you may not see a direct impact of these micronutrients on your blood sugar, you could be helping the root cause of your prediabetes.
Other herbal supplements to consider would be adaptogens that can help your body adapt to and better respond to stress such as rhodiola, berberine, and cacao flavonoids.
The book The XX Brain by Dr. Lisa Mosconi has helpful tables for different supplements to help for things like anxiety, depression, metabolism, and sleep. If you're looking for specific amounts to take per day, look in this book for reference.
Be sure to always run a supplement by your doctor before taking them because they could interfere with your current medications.
Remember though, you can never out-supplement an unhealthy lifestyle. Many lifestyle factors, not just what you eat, can impact your blood sugar. Food timing, sleep, stress, your environment or toxin exposure, and exercise are also areas you can optimize.
It does take time and effort, but your health is worth it. All of these lifestyle factors are addressed in Zivli, our online weight loss course and coaching program.
Tips to Control Your Blood Sugar After a High Carb Meal
Tip #1: Eat or Drink Fermented Foods
Apple cider vinegar is my go-to. There are two pronounced benefits of consuming fermented foods. The first is that when the bacteria ferment the food, they aren’t eating the protein and fat in the food, they are eating the starches (or sugar).
The bacteria we consume by eating fermented food or liquid digest some of the carbs first, mean we are getting less starch than the non fermented version. The other benefit is the beneficial bacteria can act as probiotics in our intestines.
Several studies have shown that having 1-2 tablespoons of apple cider vinegar with a starchy meal helps lower the glucose and insulin effect of that meal in insulin-resistant people, and may help generally improve glucose control for type 2 diabetes.
Taking two tablespoons of raw apple cider vinegar in the evening helps control glucose levels the following morning, lowering the normal “dawn effect” of elevated blood sugars from the morning rush of cortisol.
A simple habit you could start is taking 1-2 tablespoons of apple cider vinegar in the morning and evening. You can dilute it with some water if you don't like the taste.
Tip #2: Move Your Body Following a High Carb Meal
Going for a short walk after dinner can create muscle demand for glucose. The glut 4 transporter is what allows blood sugar to go from your bloodstream into your cells.
There are two primary stimulators of the glut4 transporter - muscle demand and insulin. Going for a walk helps not only reduce your immediate blood sugar, but will help reduce the amount of insulin required to take care of the carbs you just ate.
Summary and Key Takeaways to Lower Blood Sugar
#1: Stop counting points and calories.
#2: Start tracking macronutrients. It will put your food on level playing fields.
#3: Swap unhealthy refined starches and sugars with healthier alternatives.
#4: Avoid sugar-free ingredients that still raise blood sugar such maltodextrin, sucralose, saccharine, acesulfame potassium, and aspartame.
#5: Choose your fats wisely.
#6: Eat more high quality protein at each meal.
#7: Optimize your micronutrients.
The hot tips were to have 1-2 tablespoons of apple cider vinegar each morning and evening, and to move your body after a high carb meal.
Subscribe & Review
Subscribing and leaving a rating and review are important factors in helping the Reshape Your Health Podcast and the YouTube Channel reach more people. If you haven't already subscribed, please do that today.
We would also be grateful if you left a rating and review, too. In your listening app, scroll to the “Ratings and Reviews” section, then click “Write a Review” and let us know what you enjoy about our show. We appreciate you taking the time to show your support. Thank you!
Resources From This Episode
>> Join Zivli
>> Freebie: Weight Loss Mindset Audio Training

